Effective for Medicare patients with DOS March 6, 2020, clinicians can bill immediately for dates of service starting March 6, 2020. These telehealth services are paid under the Physician Fee Schedule and paid at the same amount as in-person services. Use of the telehealth modifier or place of service code would be necessary for tracking. Medicare coinsurance and deductible still apply for these services. Additionally, the HHS Office of Inspector General (OIG) is providing flexibility for health care providers to reduce or waive cost-sharing for telehealth visits paid by federal health care programs.
This week’s announcement by CMS means that physicians who want or can use audio and video communication technology to provide telehealth to patients during the COVID-19 nationwide public health emergency can use any non-public facing service that is available to communicate with patients.
This exercise of discretion applies to telehealth provided for any reason, regardless of whether the telehealth service is related to the diagnosis and treatment of health conditions related to COVID-19. Under this Notice, physicians may use popular applications that allow for video chats, including Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, or Skype to provide telehealth without risk that OCR might seek to impose a penalty for noncompliance with the HIPAA Rules.
Physicians should not use Facebook Live, Twitch, TikTok or other public facing communication services. Physicians are encouraged, but not required, to notify patients of the potential security risks of using these services and to seek additional privacy protections by entering into HIPAA business associate agreements (BAA). HHS also noted that while it hasn’t confirmed such statements, Skype for Business, Updox, VSee, Zoom for Healthcare, Doxy.me, and Google G Suite Hangouts have said that their products will help physicians comply with HIPAA and that they will enter into a HIPAA BAA.
The changes and items of note are:
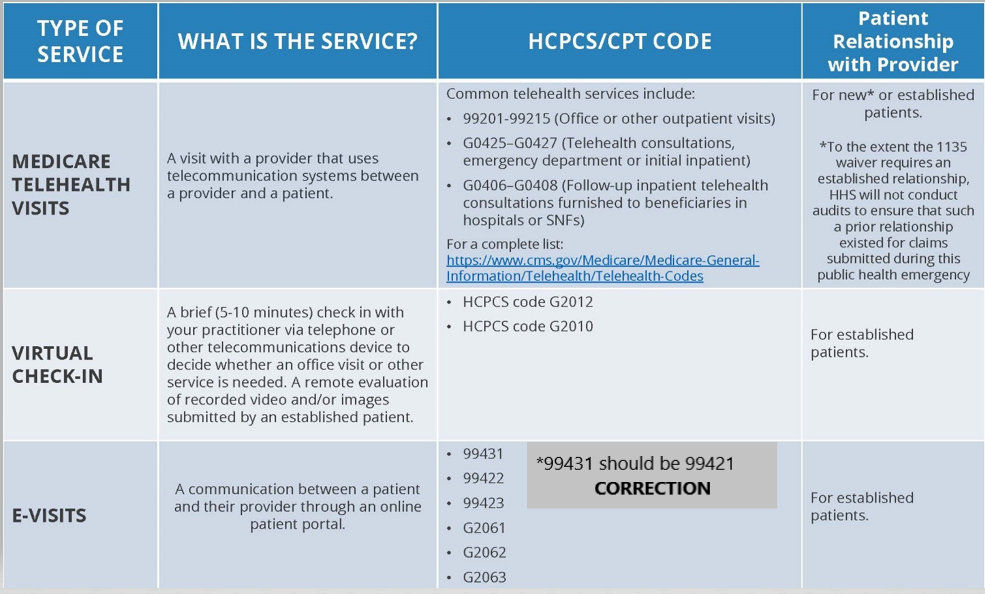
- Telehealth everywhere (i.e., office visits 99201-99215) requires video, in addition to audio; (however, video may be by non-public facing video, such as Skype as detailed above).
- Code 99201-99205, 99211-99215 (POS 02 for Telehealth [Medicare], modifier 95 [Commercial Payers]).
- Online visits, patient portals and other electronic contacts initiated by the patient; the physician services may be billed using CPT codes 99421-99423, and HCPCS codes G2061-G2063 or CPT code 98970-98972 for qualified non-physician health care professionals, as applicable.
- Telephone visit initiated by the physician or QHP are considered the brief check-in G2012.
- Providers can waive co-pays for all federal health care systems (Medicare, Medicaid, etc).
- HHS will not audit for existence of a prior relationship (i.e., typically used for established patients, but could be used for new patients at discretion).
- Applies to claims submitted during this public health emergency.
- This guidance follows on President Trump’s call for all insurance companies to expand and clarify their policies around telehealth. The ATS supports all payers expanding the options for providers’ virtual visits and consistent policies to ease provider burden and expand patient access.
To read the Fact Sheet on this announcement, please click here.
To read the Frequently Asked Questions on this announcement, please click here.
This guidance, and earlier CMS actions in response to the COVID-19 virus, are part of the ongoing White House Task Force efforts. To keep up with the important work the Task Force is doing in response to COVID-19, click here.
COVID-19 Coding guidance: ICD-10-CM
- Pneumonia:For a pneumonia case confirmed as due to the 2019 novel coronavirus (COVID-19), assign codes J12.89, Other viral pneumonia, and B97.29, Other coronavirus as the cause of diseases classified elsewhere.
- Acute bronchitis:For a patient with acute bronchitis confirmed as due to COVID-19, assign codes J20.8, Acute bronchitis due to other specified organisms, and B97.29. If the bronchitis is not specified as acute, due to COVID-19, report code J40, Bronchitis, not specified as acute or chronic, along with code B97.29.
- Lower respiratory infection:If the COVID-19 is documented as being associated with a lower respiratory infection, not otherwise specified (NOS), or an acute respiratory infection, NOS, report with code J22, Unspecified acute lower respiratory infection, with code B97.29. If the COVID-19 is documented as being associated with a respiratory infection, NOS, it would be appropriate to assign code J98.8, Other specified respiratory disorders, with code B97.29.
- Acute respiratory distress syndrome (ARDS):ARDS may develop in conjunction with COVID-19. Cases with ARDS due to COVID-19 should be assigned the codes J80, Acute respiratory distress syndrome, and B97.29.
- Exposure to COVID-19:For cases where there is possible exposure to COVID-19, but the disease is ruled out, report code Z03.818, Encounter for observation for suspected exposure to other biological agents ruled out. For cases where there is an actual exposure to someone who is confirmed to have COVID-19, report code Z20.828, contact with and (suspected) exposure to other viral communicable diseases. This code is not necessary if the exposed patient is confirmed to have COVID -19.
- Signs and symptoms:For patients presenting with any signs/symptoms and where definitive diagnosis has not been established, assign the appropriate code(s) for each of the presenting signs and symptoms such as: Cough (R05); Shortness of breath (R06.02) or Fever unspecified (R50.9).
Do not report “suspected” cases of COVID-19 with B97.29. In addition, diagnosis code B34.2, Coronavirus infection, unspecified, typically is not appropriate.